Diagnostic testing includes the basic semen analysis, the sperm penetration assay testing (SPA), testing for the presence of anti-sperm antibodies, testing for reproductive hormones, post vasectomy checks, semen cultures, and biochemical tests. Other diagnostic services include advanced genetic testing, including the evaluation of sperm and embryo chromosome aneuploidy.
Generally, the semen analysis is the “starting point” in the evaluation of male infertility and may indicate possible causes of decreased fertility and avenues of further study. The sperm penetration assay is particularly helpful in evaluating possible treatment options. Some of our more common tests are listed below:
- Semen Analysis
- Sperm Penetration Assay (Hamster Egg Penetration Test)
- Anti-sperm Antibody Test
- Retrograde Analysis
- Hormone Evaluation
- Post Vasectomy Analysis
Semen Analysis
 The semen analysis is relatively noninvasive and costs less than most female infertility tests, yet provides a general overview of the male’s fertility status. This makes it ideal for starting infertility evaluation. It may also provide insight that could lead to further testing and an accurate diagnosis of the underlying cause of reduced fertility.
The semen analysis is relatively noninvasive and costs less than most female infertility tests, yet provides a general overview of the male’s fertility status. This makes it ideal for starting infertility evaluation. It may also provide insight that could lead to further testing and an accurate diagnosis of the underlying cause of reduced fertility.
For regulatory purposes, there must be a written physician’s order before obtaining a semen analysis in our laboratory. After our staff receives the order a semen analysis may be scheduled by calling 612-863-4115 and requesting a laboratory appointment.
To obtain accurate test results it is necessary to abstain from sexual activity for two to seven days before the appointment. A shorter period of abstinence may affect sperm concentration while a longer period may diminish sperm motility.
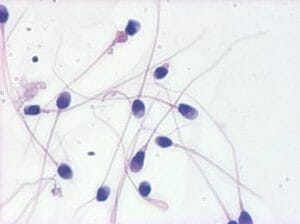
The evaluation of the sperm includes a determination of the sperm concentration, progressively motile sperm count, and sperm morphology (shape). Decreases in sperm concentration and sperm motility affect the motile sperm count, which reflects the ability to get a high enough concentration of sperm to the egg site to complete fertilization. Sperm morphology is important because it too may reflect upon the ability of the sperm to fertilize an egg, as well as underlying spermatogenesis defects. Abnormal sperm morphology usually does not reflect the potential for risk to offspring. In fact, using current guidelines a normal semen sample may consist of only 4% or greater of morphologically normal sperm. A smaller percentage of normal sperm may reflect a reduced fertility.
Sperm viability, or the percentage of viable sperm, may be determined using either “membrane-exclusion dyes” or the “hypoosomatic solution assay” (HOS). These tests examine the sperm’s plasma membrane and its ability to function normally, as well as potentially flagging some pathologies that may include damage to the sperm membrane. The seminal fluid’s viscosity is evaluated in relation to sperm motility. Sperm agglutination, or the tendency for the sperm to stick together, may indicate the presence of anti-sperm antibodies. It is normal for the seminal fluid to have a small number of white blood cells, but an increased presence of these cells may indicate an infection or prostatitis (inflammation of the prostate). If the white blood cell count necessitates a semen culture, a diagnosis and treatment for the problem may be found.
If no sperm are found in the seminal fluid, an evaluation of fructose will be performed. A lack of fructose may indicate a blockage of the vas deferens, which secretes fructose and carriers the sperm from the epididymis to the prostate gland.
Sperm Penetration Assay (Hamster Egg Penetration Test)
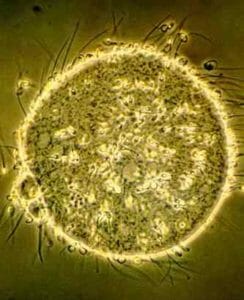
The use of the sperm penetration assay (SPA) as a measure of sperm fertilizing ability is based on the theory that sperm that undergo the preliminary chemical steps necessary for normal fertilization can also penetrate chemically-modified hamster ova, which can be observed under the microscope. Removal of the zona pellucida on hamster oocytes will allow penetration by human sperm in vitro. For penetration to occur, the sperm must be able to undergo capacitation, the acrosome reaction, oolemma fusion, and incorporation into the ooplasm. Therefore sperm treated similar to IVF sperm preparation can be evaluated for fertilization capacity.
 The sperm penetration assay is the most accurate test to predict the ability of sperm to fertilize an egg. It also aids in determining if laboratory techniques might improve the sperm’s ability to fertilize, or if intracytoplasmic sperm injection (ICSI) should be used during IVF therapy.
The sperm penetration assay is the most accurate test to predict the ability of sperm to fertilize an egg. It also aids in determining if laboratory techniques might improve the sperm’s ability to fertilize, or if intracytoplasmic sperm injection (ICSI) should be used during IVF therapy.
The prepared sperm are incubated with 10-15 hamster eggs. If functionally competent, the human sperm can complete the first steps of fertilization including the penetration of the egg, but nothing happens beyond that point. The penetrated eggs are counted and a percentage is calculated.
When test results are evaluated; if less than 50 percent of the eggs are penetrated in the non-stimulated sperm, there is a decreased ability to fertilize. A percentage higher than 50 indicates that the sperm should have the ability to fertilize. An unstimulated sample with a penetration rate between 30 percent and 50 percent sperm may indicate that stimulation of the sample may improve fertilization during artificial insemination. If a sample has a 30 percent or less penetration rate the likelihood of a sperm defect is high and intracytoplasmic sperm injection (ICSI) joined by IVF is usually recommended.
Anti-Sperm Antibody Test
In males, a “blood-testis” barrier exists that immunologically protects sperm from the man’s own immune system. This is to keep the body from identifying the sperm as foreign, classifying it as dangerous and producing antibodies against the sperm. When these barriers break down, the body produces anti-sperm antibodies. If these antibodies attach themselves to sperm they cause severely diminished motility and/or cause sperm agglutination. The presence of antibodies is evaluated by testing seminal fluid, semen, and/or serum. There should be an anti-sperm antibody evaluation performed in cases where sperm motility is diminished and/or in samples with an increase of agglutination or reduced sperm viability. Females may also produce anti-sperm antibodies. Females should be evaluated if when the physician determines that it is necessary.
Retrograde Analysis
A retrograde semen analysis is indicated for patients with a low semen volume and/or alter seminal fluid pH and azoospermia in the initial semen analysis. Retrograde ejaculation is the ejaculation of sperm into the bladder. Urine voided following sexual activity will contain sperm in men who undergo retrograde ejaculation. Many retrograde ejaculation patients will have had prior surgery or a medical condition that predisposes them to retrograde ejaculation. Predisposing factors include testicular cancer surgery (RPLND), transurethral surgery of the prostate, or childhood bladder surgery. Medical conditions such as diabetes, MS, or spinal cord injury may also predispose an individual to retrograde ejaculation.
Hormone Evaluation
If no sperm are found in the semen, or if the count is extremely low, a blood sample may be obtained for the purpose of evaluating the levels of follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone, and prolactin. Clues from these tests may lead to probable causes and appropriate therapies.
Post Vasectomy Analysis
This test serves as an indicator of the status of an individual’s vas deferens patency following a vasectomy. The sample is evaluated for the presence or absence of spermatozoa. If non-motile sperm are present, it may indicate that additional ejaculations are required to fully clear the reproductive tract of sperm. At least 4-5 weeks should elapse after the vasectomy is performed before testing. Several post vasectomy analyses may be needed. The number of samples collected following a vasectomy is under the physician’s direction.